Wednesday, November 30, 2016
Cellulitis vs. Abscess
Cellulitis is a diffuse infection of the soft tissues with no localized area of pus amenable to drainage. The affected area is described as indurated (i.e., warm, red, and swollen). It is also painful. A component of lymphangitis (infection involving the lymphatics) is indicated by red streaking, progressing proximally from the affected area.
An abscess is a localized collection of pus, often with a component of surrounding cellulitis (with the above signs). One sign of an abscess is an area of fluctuance; that is, when you apply gentle digital pressure over the area, you can push and feel a “give,” indicating the presence of fluid underneath. Another sign is that an abscess often seems to “point;” that is, the skin starts to thin from the pressure of the fluid underneath. The distinction between cellullitis and abscess is important. The main treatment for an abscess is incision and drainage (cutting into the abscess and widely opening the abscess cavity). Cellulitis does not warrant this intervention.
skin infxn
http://www.forbes.com/sites/judystone/2015/03/18/choosing-an-antibiotic-for-skin-infections-whats-best/#197415c17065
antibiotics
Source: http://www.microbiologynutsandbolts.co.uk/the-bug-blog/-how-to-remember-antibiotic-spectrums-of-activity
I am often asked “how can doctors remember the different
antibiotic spectrums of activity”? This is a difficult task as there are so many. Personally I have never found lists of medical information that helpful, I would much rather come up with a mnemonic. However, I’m stumped for a mnemonic to remember antibiotic spectrum of activity, so a list it must be. What I have done though is reduce a very long list into six short related lists, which I hope are easier to remember.
antibiotic spectrums of activity”? This is a difficult task as there are so many. Personally I have never found lists of medical information that helpful, I would much rather come up with a mnemonic. However, I’m stumped for a mnemonic to remember antibiotic spectrum of activity, so a list it must be. What I have done though is reduce a very long list into six short related lists, which I hope are easier to remember.
NOT knowing the spectrum of activity of the antibiotic they are prescribing is high up there on the list of situations when doctors make a mistake. NOTknowing leads to patients being given antibiotics which have no activity against the bacteria which are known or suspected to be the cause of an infection. My current pet hate is the use of Teicoplanin to treat UTIs (see Teicoplanin blog...) but I also come across patients being treated for Pseudomonas spp. with Co-amoxiclav which has no activity against Pseudomonas spp., or an anaerobic infection being treated with both Co-amoxiclav AND Metronidazole when either alone would be enough. Sometimes it seems doctors are just guessing or picking their favourites!
Remembering the 6 lists below will help to ensure patients are on an antibiotic that is active against their infection.
Lists 1 and 2
Remembering the 6 lists below will help to ensure patients are on an antibiotic that is active against their infection.
- Active against Gram-positive and Gram-negative bacteria (Broad-spectrum antibiotics)
- Active against anaerobes
- Active against Pseudomonas spp.
- Active ONLY against Gram-positive bacteria
- Active ONLY against Gram-negative bacteria
- Active against “non-culturable” bacteria
Lists 1 and 2
Example A: A patient has a perforated appendix. Which antibiotics could be used to cover the mixed bowel flora that will have leaked into the patient’s peritoneum? Any of Co-amoxiclav, Piptazobactam, Ertapenem, Imipenem or Meropenem could be used alone as they are broad spectrum AND cover anaerobes. If Cefuroxime, Ceftriaxone or Cefotaxime were used then Metronidazole would need to be added to cover the anaerobes. You would not use Cefuroxime, Ceftriaxone or Cefotaxime with Clindamycin as this poses too high a risk for Clostridium difficile associated diarrhoea (CDAD).
Example B: In patients with serious penicillin allergies Beta-lactams including Co-amoxiclav, Piptazobactam, Ertapenem, Imipenem or Meropenem are contraindicated. Combinations of antibiotics are therefore needed to cover the gut flora, such as Teicoplanin OR Vancomycin (which only have Gram-positive activity) PLUS Metronidazole (which only covers anaerobes) PLUS either Ciprofloxacin ORGentamicin (both of which have excellent Gran-negative activity).
List 3
Example B: In patients with serious penicillin allergies Beta-lactams including Co-amoxiclav, Piptazobactam, Ertapenem, Imipenem or Meropenem are contraindicated. Combinations of antibiotics are therefore needed to cover the gut flora, such as Teicoplanin OR Vancomycin (which only have Gram-positive activity) PLUS Metronidazole (which only covers anaerobes) PLUS either Ciprofloxacin ORGentamicin (both of which have excellent Gran-negative activity).
List 3
Example C: A Cystic Fibrosis (CF) patient has an exacerbation of their CF caused by Pseudomonas aeruginosa. What antibiotics would they be treated with? They would be treated with a combination of antibiotics active against Pseudomonas aeruginosasuch as IV Meropenem PLUS IV Tobramycin PLUSnebulised Colistin.
Why a combination of antimicrobials? Combination antimicrobials are used to try and prevent further development of resistance (Pseudomonas aeruginosais notorious for acquiring new resistance mechanisms), in non-CF patients two antimicrobials are usually enough. It is unlikely that bacteria will become resistant to two or more antimicrobials at the same time therefore resistance is less likely to occur. Even if the bacteria do become resistant to
one of the antimicrobials the other agent(s) will be able to kill the bacteria.
List 4 and 5
Why a combination of antimicrobials? Combination antimicrobials are used to try and prevent further development of resistance (Pseudomonas aeruginosais notorious for acquiring new resistance mechanisms), in non-CF patients two antimicrobials are usually enough. It is unlikely that bacteria will become resistant to two or more antimicrobials at the same time therefore resistance is less likely to occur. Even if the bacteria do become resistant to
one of the antimicrobials the other agent(s) will be able to kill the bacteria.
List 4 and 5
Example D: A patient has a skin and soft tissue infection but also has a severe allergy to penicillins. Which antibiotics could be used to treat them? Skin and soft tissue infections are almost always caused by Gram-positive bacteria such as Staphylococcus aureus or Beta-haemolytic streptococci therefore Vancomycin, Teicoplanin, Linezolid and Daptomycin would all be capable of treating the infection. It may sound obvious but you cannot use an antimicrobial only active against Gram-negatives to treat a Gram-positive, therefore Ceftazidime, Colistin or Aztreonam would definitely not be appropriate as they do not have any activity against the Gram-positive causes. Broad-spectrum antibiotics would treat the infection but it would be unnecessary as the bacteria are known to be Gram-positive. Broad spectrum antibiotics in this case might lead to unwanted side effects such as CDAD.
List 6
List 6
Example E: A patient has pneumonia caused by Mycoplasma
pneumoniae (a non-culturable bacterium). What antibiotic should they be treated with? Erythromycin, Clarithromycin, Azithromycin, Ciprofloxacin, Levofloxacin and Doxycycline all could be used to treat this patient.
If you can learn these six lists it starts to become much easier to understand why certain antibiotics are chosen to treat certain infections. It also enables you to choose alternatives when patients are allergic to first line antibiotics found in guidelines. Downloada handy postcard of the 6 lists and keep it in your book Microbiology Nuts and Bolts.
Give it a try and see if it helps. Pass it on too. If you can think of any easy way of remembering them then let me know, I’m always keen to know how others have learned their microbiology.
pneumoniae (a non-culturable bacterium). What antibiotic should they be treated with? Erythromycin, Clarithromycin, Azithromycin, Ciprofloxacin, Levofloxacin and Doxycycline all could be used to treat this patient.
If you can learn these six lists it starts to become much easier to understand why certain antibiotics are chosen to treat certain infections. It also enables you to choose alternatives when patients are allergic to first line antibiotics found in guidelines. Downloada handy postcard of the 6 lists and keep it in your book Microbiology Nuts and Bolts.
Give it a try and see if it helps. Pass it on too. If you can think of any easy way of remembering them then let me know, I’m always keen to know how others have learned their microbiology.
Choosing Antibiotics
From: https://firstaidteam.com/2014/01/13/wards-survival-series-everything-you-need-to-know-about-antibiotics-a-3-part-series/
Wards Survival Series: Wards Survival Series & USMLE Study Tips: Choosing Antibiotics
By Michael Spinner
Choosing the right antibiotics to treat an infection can be a daunting task for medical students given the sheer number of different drugs, infections, and organisms we have to memorize. However, a strong understanding of antibiotics is critical as they are some of the most commonly prescribed medications as well as a very common source of questions on boards exams and pimping on the wards. In this post, we offer some useful tips to help guide you as you think about choosing the right antibiotics to treat infections.
When thinking about how to treat an infection, first consider the likely causative organism. Is the organism likely bacterial, viral, fungal, or parasitic? Remember that antibiotics are only indicated to treat bacterial infections (with a few exceptions like metronidazole which also has excellent anti-protozoal coverage). The vast majority of upper respiratory infections and some lower respiratory infections (e.g. acute bronchitis) are caused by viruses and thus do not require treatment with antibiotics. Remembering this simple fact will help you to avoid exposing patients to unnecessary side effects and prevent antibiotic resistance.
In the case of a likely bacterial infection, first consider which of the following broad groups of bacteria are the most likely culprits: gram-positives, gram-negatives, anaerobes, and/or atypicals. For community-acquired pneumonia, the most common causative organisms are gram-positive (e.g. Streptococcus pneumoniae) or atypical bugs like Mycoplasma, Chlamydia, and Legionella. Thus, an appropriate antibiotic would cover both gram-positive and atypical organisms, making azithromycin an excellent choice. For appendicitis or diverticulitis, you should cover empirically for colonic anaerobes and gram-negative enterics, making piperacillin/tazobactam an appropriate agent.
Grouping bacteria into these four broad groups is a great place to start when thinking about antibiotic coverage. However, memorizing the specific antibiotics that cover certain bugs (especially MRSA and Pseudomonasaeruginosa) can be high-yield for board exams and on the wards. A list of the antibiotics that cover MRSA and Pseudomonas is provided below:
MRSA coverage Pseudomonas coverage
Vancomycin Piperacillin/tazobactam
Clindamycin Cefepime, ceftazidime
Doxycycline Carbapenems (except ertapenem)
TMP/SMX Aztreonam
Linezolid Aminoglycosides
Daptomycin Fluoroquinolones
Vancomycin Piperacillin/tazobactam
Clindamycin Cefepime, ceftazidime
Doxycycline Carbapenems (except ertapenem)
TMP/SMX Aztreonam
Linezolid Aminoglycosides
Daptomycin Fluoroquinolones
In addition to considering the likely causative organism, also consider the source of infection. If the antibiotic does not adequately reach the source then its coverage won’t matter! For example, both doxycycline and vancomycin cover MRSA, but the preferred treatment depends on the source. Oral doxycycline is a reasonable choice to treat MRSA cellulitis but would not be an appropriate choice for MRSA bacteremia or osteomyelitis. A bloodstream MRSA infection would require treatment with an intravenous agent like vancomycin. Similarly, treating meningitis requires an agent with good CSF penetration like ceftriaxone.
Last, be sure to consider the side effects. Aminoglycosides and vancomycin are nephrotoxic and should be avoided in renal failure. Numerous antibiotics have adverse effects in utero and should be avoided in pregnancy. Penicillin and sulfa allergies are extremely common and will often affect antibiotic choices.
As with reading a chest X-ray or EKG, having a systematic approach to choosing antibiotics will help you to approach this topic with confidence on the wards and board exams. Whether you’re studying for Step1 or Step 2 or just trying to survive on the wards, I hope that these pointers will serve you well!
Saturday, November 26, 2016
Progestorone, Progestin, Progestogen
source: http://womeninbalance.org/resources-research/bioidentical-progesterone-vs-synthetic-progestins/
Confusion exists, even among leading experts in the field of hormone research, between the terms progesterone, progestin, and progestogen. Although these terms are often used interchangeably, they are not synonymous.
Confusion exists, even among leading experts in the field of hormone research, between the terms progesterone, progestin, and progestogen. Although these terms are often used interchangeably, they are not synonymous.
Until an authoritative definition is formally adopted, the following reflects the current culture of the usage of these terms, and clarifies how they are used by Women in Balance: “progesterone” refers to the hormone produced in the body, or produced from a plant source but still chemically and structurally identical to human progesterone, and it is therefore referred to as “bioidentical” or “natural”.
In contrast, “progestin” refers to a hormone that is synthetically produced and differs in structure from progesterone. There are numerous synthetic progestins used in hormone therapy, in contrast to only one molecule referred to as progesterone. “Progestogen” (sometimes spelled “progestagen”) is a general term for hormones that act like progesterone in the uterus, and therefore includes both progesterone and progestins.
There is increasing evidence that, by virtue of their different chemical structures, synthetic progestins do not always act as progesterone would at the same target tissues. This has long been understood with respect to treatment of pregnancy and fertility issues, when progesterone is effectively prescribed, yet synthetic progestins are contraindicated.
While synthetic progestins may mimic some of progesterone’s effects, progestins may react differently with progesterone receptors in the body. A significant consequence of the side effects seen with synthetic progestins has been an increase in the risk of developing breast cancer. Clinical trials such as the Women’s Health Initiative, in which more breast cancer was seen in the group taking progestins, did not study natural progesterone
Wednesday, November 23, 2016
oral sex & yeast infxn
http://www.webmd.com/women/news/20031219/yeast-infections-not-mens-fault
Dec. 19, 2003 -- Specific sex practices -- and not infection in men -- are linked to women's recurring yeast infections, a new study shows.
Those sex practices -- oral sex performed on a woman and masturbation with saliva -- don't actually spread yeast infections, researchers report. Instead, they may in some women create conditions that let yeast grow out of control.
University of Michigan researcher Barbara D. Reed, MD, MSPH, led the study of 148 women and 78 of their male sex partners.
"Many physicians -- and many women -- believe that women get recurrent yeast infections because their partner passes the yeast back to them during intercourse. This study refutes that belief," Reed says in a news release.
All of the women originally were treated for candidayeast infections. Reed's team collected culture samples from the women's tongue, feces, vulva, and vagina and from their sex partners' tongue, feces, urine, and semen.
The women had check-ups at two weeks, four weeks, six months, and a year -- as well as whenever they had a yeast infection. Whenever a woman had symptoms of a yeast infection, her sex partner was checked as well.
Yeast can live peacefully in the vagina without overgrowing and causing the intense itching and burning that indicate candida vulvovaginitis or yeast infection. Reed's team confirmed this. Women found to have yeast in their vaginas during follow-up visits were no more likely than other women to have recurring symptoms of yeast infection.
Detection of yeast in male sex partners had nothing to do with whether women had recurring yeast infections.
However, sex behaviors showed a strong connection. Cunnilingus -- oral sex performed on a woman -- tripled the women's risk of recurring yeast infections. And masturbation with saliva -- both by women and by their sex partners -- doubled women's risk of recurring yeast infection.
Reed and colleagues suggest that a delicate balance exists between yeast, normal vaginal bacteria, and vaginal immune mechanisms.
"We suggest that the effects of genital washing with saliva -- from either the male or the female -- might upset this balance," they write in the December issue of the Journal of Women's Health.
The study also showed two other things that increase a woman's risk of recurring yeast infections: Eating two or more servings of bread each day, and their male sex partners who first had sex at an early age. It's not yet entirely clear how these factors play a role in yeast infections.
macrobid vs macrodantin
from: https://www.goodrx.com/blog/macrobid-vs-macrodantin-whats-the-difference/
Macrobid vs Macrodantin: What’s the Difference?
by The GoodRx Pharmacist on September 16, 2015 at 3:04 pm
Macrobid and Macrodantin look alike and sound alike—down to having almost the same active ingredient. They’re both used to treat urinary tract infections, but there are a few key differences you may want to keep in mind.
Macrobid has its daily dosing schedule right in its name—it’s taken 2 times daily (sometimes abbreviated BID on a prescription: MacroBID). The active ingredient in Macrobid is nitrofurantoin monohydrate macrocrystals or nitrofurantoin mono/macro.
Macrodantin, on the other hand, is typically taken 4 times daily. The active ingredient in Macrodantin is nitrofurantion macrocrystalline (sometimes just referred to as nitrofurantoin)—which differs a little from the type of nitrofurantoin in Macrobid.
How is Macrodantin (nitrofurantoin macrocrystalline) available?
Macrodantin is available as a capsule in three strengths: 25 mg, 50 mg, and 100 mg.
What are macrocrystals?
Nitrofurantoin products were originally formulated as microcrystals, which came with the unwanted side effects of nausea and vomiting. Medications containing nitrofurantoin were later reformulated with macrocrystals to slow absorption and decrease the effect on your stomach. Only the macrocrystalline versions are still available.
Nitrofurantoin products were originally formulated as microcrystals, which came with the unwanted side effects of nausea and vomiting. Medications containing nitrofurantoin were later reformulated with macrocrystals to slow absorption and decrease the effect on your stomach. Only the macrocrystalline versions are still available.
Macrobid takes this a step further by using the monohydrate salt form—all you need to know about this is that it is supposed to further decrease the chance of stomach upset.
Is there an advantage to using Macrobid instead of Macrodantin?
Yes. Macrobid may be easier to take, since it’s given twice daily (while Macrodantin needs to be taken four times daily). Medications like Macrodantin that are taken more frequently throughout the day have a much smaller chance of you taking them as prescribed.
As mentioned above, you may also have a smaller chance of an upset stomach with Macrobid.
How do they compare in price?
Macrobid comes away with a clear advantage here too, at almost half the price of Macrodantin.
Macrobid comes away with a clear advantage here too, at almost half the price of Macrodantin.
Both are available as generics, and the recommended course is usually one week to start with. This means you would take 28 capsules of Macrodantin (4 times daily) and only 14 capsules of Macrobid (2 times daily).
| Pharmacy | Cash Price | GoodRx Price |
|---|---|---|
| CVS | $41 | $19 |
| Rite-Aid | $53 | $25 |
| Walgreens | $48 | $26 |
| Walmart | $50 | $32 |
| Pharmacy | Cash Price | GoodRx Price |
|---|---|---|
| CVS | $61 | $40 |
| Rite-Aid | $118 | $45 |
| Walgreens | $77 | $42 |
| Walmart | $69 | $46 |
*Prices as of September 16, 2015.
nitrofurantoin
From: http://www.rxlist.com/macrobid-drug/clinical-pharmacology.htm
CLINICAL PHARMACOLOGY
Each Macrobid capsule contains two forms of nitrofurantoin. Twenty-five percent is macrocrystalline nitrofurantoin, which has slower dissolution and absorption than nitrofurantoin monohydrate. The remaining 75% is nitrofurantoin monohydrate contained in a powder blend which, upon exposure to gastric and intestinal fluids, forms a gel matrix that releases nitrofurantoin over time. Based on urinary pharmacokinetic data, the extent and rate of urinary excretion of nitrofurantoin from the 100 mg Macrobid capsule are similar to those of the 50 mg or 100 mg Macrodantin® (nitrofurantoin macrocrystals) capsule. Approximately 20-25% of a single dose of nitrofurantoin is recovered from the urine unchanged over 24 hours.
Plasma nitrofurantoin concentrations after a single oral dose of the 100 mg Macrobid capsule are low, with peak levels usually less than 1 mcg/mL. Nitrofurantoin is highly soluble in urine, to which it may impart a brown color. When Macrobid is administered with food, the bioavailability of nitrofurantoin is increased by approximately 40%.
Microbiology
Nitrofurantoin is a nitrofuran antimicrobial agent with activity against certain Gram-positiveand Gram-negative bacteria.
Mechanism of Action
The mechanism of the antimicrobial action of nitrofurantoin is unusual among antibacterials. Nitrofurantoin is reduced by bacterial flavoproteins to reactive intermediates which inactivate or alter bacterial ribosomal proteins and other macromolecules. As a result of such inactivations, the vital biochemical processes of protein synthesis, aerobic energy metabolism, DNA synthesis, RNA synthesis, and cell wall synthesis are inhibited. Nitrofurantoin is bactericidal in urine at therapeutic doses. The broad-based nature of this mode of action may explain the lack of acquired bacterial resistance to nitrofurantoin, as the necessary multiple and simultaneous mutations of the target macromolecules would likely be lethal to the bacteria.
Interactions with Other Antibiotics
Antagonism has been demonstrated in vitro between nitrofurantoin and quinolone antimicrobials. The clinical significance of this finding is unknown.
Development of Resistance
Development of resistance to nitrofurantoin has not been a significant problem since its introduction in 1953. Cross-resistance with antibiotics and sulfonamides has not been observed, and transferable resistance is, at most, a very rare phenomenon.
Nitrofurantoin has been shown to be active against most strains of the following bacteria both in vitro and in clinical infections [see INDICATIONS AND USAGE):
Sunday, November 20, 2016
pyridium
Side effects[edit]
Phenazopyridine produces a vivid color change in urine, typically to a dark orange to reddish color. This effect is common and harmless, and indeed a key indicator of the presence of the drug in the body. Users of phenazopyridine are warned not to wear contact lenses, as phenazopyridine has been known to permanently discolor contact lenses and fabrics.[1][5]
Phenazopyridine can also cause headaches, upset stomach (especially when not taken with food), or dizziness. Less frequently it can cause a pigment change in the skin or eyes, to a noticeable yellowish color. This is due to a depressed excretion via the kidneys causing a buildup of the drug in the skin, and normally indicates a need to discontinue usage.[2] Other such side effects include fever, confusion, shortness of breath, skin rash, and swelling of the face, fingers, feet, or legs.[1][2] Long-term use may cause yellowing of nails.[6]
Phenazopyridine should be avoided by people with glucose-6-phosphate dehydrogenase deficiency,[2][7][8][9] because it can cause hemolysis (destruction of red blood cells) due to oxidative stress.[10] It has been reported to cause methemoglobinemia after overdose and even normal doses.[11] In at least one case the patient had pre-existing low levels of methemoglobin reductase,[12] which likely predisposed her to the condition. It has also been reported to cause sulfhemoglobinemia.[2][13][14] [15]
Phenazopyridine is an azo dye.[16][17] Other azo dyes, which were previously used in textiles, printing, and plastic manufacturing, have been implicated as carcinogensthat can cause bladder cancer.[18] While phenazopyridine has never been shown to cause cancer in humans, evidence from animal models suggests that it is potentially carcinogenic.[2][19]
Saturday, November 19, 2016
Friday, November 18, 2016
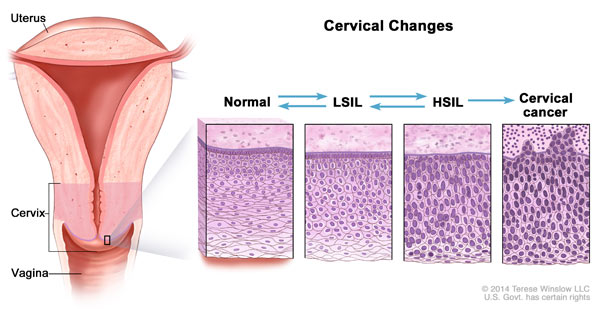
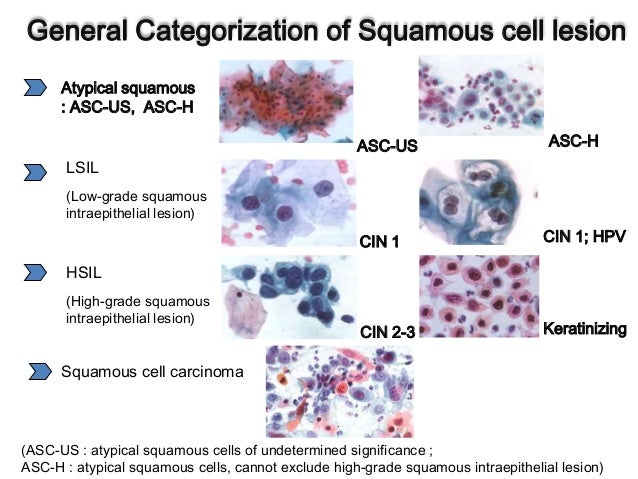
ASC-H
Squamous cells from the cervix - looking at them under the microscope and they're looking at the cell. Nowadays, they can do it thru computer, no longer under the microscope. It is actually a pre-cancerous. They need to see if it looks abnomal. You don't have to know the details but they look very werid. You can have abnormal cells of unknown significance. Low grade, high grade and then canceous. There are other scoring systems too.
Low grade is not as bad as high grade.
If they look at the cells, they're normal. We're trying to determine if it's normal or not. There are various factors. Shapes of the cells. It's not black and white. It's not on and off. There's gradient from normal to abnormal. There's structure scoring system
Low grade is not as bad as high grade.
If they look at the cells, they're normal. We're trying to determine if it's normal or not. There are various factors. Shapes of the cells. It's not black and white. It's not on and off. There's gradient from normal to abnormal. There's structure scoring system
Wednesday, November 16, 2016
Monday, November 7, 2016
Pantry
Dry goods:
- PASTA/NOODLES: different kinds of pasta, some rice, some oats, some dry beans and
lentils. Quinoa, and quinoa is a high protein grain that's also high
in fiber.
- Flour on hand for baking: baking powder, and a little bit of sugar on hand, for days when you feel like baking something. I also love using nut flours, like almond meal and hazelnut flour. But if you're not a big fan
- Nuts: different kinds of nuts and some dried fruit in your food cupboard.
- SPICE: chili powder, coriander, black pepper, and dried thyme. There's a bottle of vanilla essence in
there too, for days when I want to bake.
- Onions, garlic, and potatoes in a dark cupboard near my pots and pans. Apparently keeping them in a dark place prevents them from sprouting, at least for a week or so.
- Fridge: eggs, some milk, butter, cheese, and yogurt in it. Carrots and tomatoes
in the vegetable drawer, and some frozen peas in the freezer.
- In some places you can actually order a farm box to be delivered to your door every week, from
a local farm. It's kind of an automatic way to increase the variety in your diet. And it's also surprisingly affordable.
=> you can make a simple pasta dish with a tomato sauce and some sprinkled cheese. You can make a quinoa salad with chopped carrots and some fresh lemon juice, or lentils and rice, or
beans and rice.
And you can dress these up with your favorite spices and flavor them with
onions and garlic.
For breakfast, you can always make oatmeal or scrambled eggs if you're in a pinch, and you can make pancakes, cakes, or cookies for occasional treats.
Now another benefit of storing some non-perishable food items in
your kitchen, is that you can buy in bulk, and sort of stock up when these
foods are on special at the supermarket. So you end up actually saving money on
your meals. Remember that even if you only have time
to boil some pasta and sprinkle some grated
cheese on top, and maybe cut up a fresh fruit, that meal
will almost certainly be healthier for your
family than a fast food dinner. My mom used to say, it's better to be real
than to be perfect. You don't need to cook like Julia Child in
order to feed your family well. Even Julia Child emphasized fearlessness
in the kitchen. One of her most famous quotes was this.
She said, learn how to cook, try new recipes, learn from your mistakes, be
fearless, and above all, have fun.
- PASTA/NOODLES: different kinds of pasta, some rice, some oats, some dry beans and
lentils. Quinoa, and quinoa is a high protein grain that's also high
in fiber.
- Flour on hand for baking: baking powder, and a little bit of sugar on hand, for days when you feel like baking something. I also love using nut flours, like almond meal and hazelnut flour. But if you're not a big fan
- Nuts: different kinds of nuts and some dried fruit in your food cupboard.
- SPICE: chili powder, coriander, black pepper, and dried thyme. There's a bottle of vanilla essence in
there too, for days when I want to bake.
- Onions, garlic, and potatoes in a dark cupboard near my pots and pans. Apparently keeping them in a dark place prevents them from sprouting, at least for a week or so.
- Fridge: eggs, some milk, butter, cheese, and yogurt in it. Carrots and tomatoes
in the vegetable drawer, and some frozen peas in the freezer.
- In some places you can actually order a farm box to be delivered to your door every week, from
a local farm. It's kind of an automatic way to increase the variety in your diet. And it's also surprisingly affordable.
=> you can make a simple pasta dish with a tomato sauce and some sprinkled cheese. You can make a quinoa salad with chopped carrots and some fresh lemon juice, or lentils and rice, or
beans and rice.
And you can dress these up with your favorite spices and flavor them with
onions and garlic.
For breakfast, you can always make oatmeal or scrambled eggs if you're in a pinch, and you can make pancakes, cakes, or cookies for occasional treats.
Now another benefit of storing some non-perishable food items in
your kitchen, is that you can buy in bulk, and sort of stock up when these
foods are on special at the supermarket. So you end up actually saving money on
your meals. Remember that even if you only have time
to boil some pasta and sprinkle some grated
cheese on top, and maybe cut up a fresh fruit, that meal
will almost certainly be healthier for your
family than a fast food dinner. My mom used to say, it's better to be real
than to be perfect. You don't need to cook like Julia Child in
order to feed your family well. Even Julia Child emphasized fearlessness
in the kitchen. One of her most famous quotes was this.
She said, learn how to cook, try new recipes, learn from your mistakes, be
fearless, and above all, have fun.
6 ingredients for every kitchen
1 - Olive oil: more expensive one for your salads, cheaper one for cooking
2 - Salt: good for your salty tongue receptors!
3 - Lemons/Limes: good for your sour tongue receptors!
4 - Onion
5 - Garlic
6 - nice-looking meats
=> enough to make a meals!
2 - Salt: good for your salty tongue receptors!
3 - Lemons/Limes: good for your sour tongue receptors!
4 - Onion
5 - Garlic
6 - nice-looking meats
=> enough to make a meals!
Processed foods
Highly processed foods have a lot of ingredients.
Less processed foods have fewer ingredients.
Buy the one with fewer ingredients
Processed foods mean anything that canned or packaged.
Wednesday, November 2, 2016
CHF
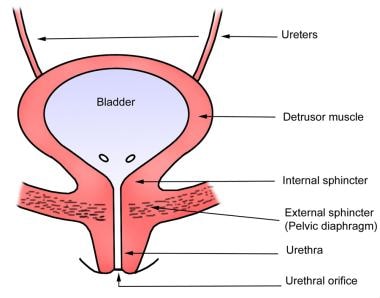
CHF is caused by fluid overload in the heart and. CHF is totally different from COPD. COPD is all about the lungs. Why is it called congestive heart failure? Because it's so much fluid. What kills HF pt? How does it kill the pt? It's the hypoxia. The real immediate problem is hypoxia, not fluid overload. It's not how much fluid int the body but it's how much fluid in the lungs. When the pt is having HF, that's the main problem. Why is there fluid in the lungs? Congestion means it's referring to the lungs. If you do a CXRAY, you'll see big heart. What's congestion? What do you see on cxray? You'll see big heart but that's not important, what's important? FLUID IN THE LUNGS. You'll see pulmonary edema = fluid overload/cushiness/leaking out in the lungs. Pulmonary edema = that's what you'll see. When CHF pt comes in, the real problem is hypoxia. You can help solve that and makes that better by giving oxygen. But ultimately, you also have to know the root cause. And, the root cause or the cause is pulmonary edema. PULMONARY EDEMA. So, what we need to know is then to get the fluid out of hte lungs. When the pt is SOB and hypoxic, do you care about getting the fluid out of the legs? NO, you care about getting the fluids out of the lungs: you want to get the pt's legs down ont he ground. Is it going to get their fluid in the legs worse? Yes. What's the problem? The LEFT ventricle. The left ventricle takes blood from the lungs and sends to the rest of the body. The right ventricle tkes blood from the rest of the body and sends it to the lungs. So, CHF, we have blood going to the lungs but we can't pump it out. There's fluid in lungs. Our main problem is the Left ventricle is not strong enough to pump fluid out. So if pt has CHF, FLUID IN THE LUNGS = HYPOXIC. And, if I make the Rt ventricle stronger, will that make the problem better or worse? worse. They may have some weakness in the Rt ventricle but the main problem is the Left ventricle is not effective enuf to pump the blood out. So, the way we can treat that is that we can make the heart stronger. This is a temporary fix. Slowing the gas pedal when the engine is already not doing so well. So, the meds like digoxin and dopamine and dobutamine will stimulate the heart and cause the heart to pump more out. If the heart is okay, it will regulate itself and it will try to push the left side harder to get that fluid out. So, how do we address it otherwise? We give them meds that cause pulling blood in the legs? Stand them up, put the legs down, use gravity. You can give the NTG. What does NTG do? It's a vasodilator. If I vasodilate my peripheral vein, what does that do? I pull more fluid out. It will only go so far tho. Bc you didn't get rid of any fluid in the body but you just move it around to somewhere else. How do I get the fluid out of the body? You actually have to use diuretics. If there's less fluid in the body, there's more fluid going to the Rt ventricle or what? Less. The Rt ventricle is going to pump less. And, the Lt ventricle job easier or harder? Easier.
What's the most common cause of CHF? HTN is a common cause. Sure. What else? too much IV fluid - might be a cause acutely in a pt in a hospital and unable to control their fluid bc their doctor/nurse is giving too much fluid but usuaully not in the world. Why does the pt have a weak heart? Not smoking but smoking makes it worse. Kidney failure? pretty close. CORONARY ARTERY DISEASE due to recurrent MI and hyperlipidemia. The 2 most common causes of CHF = CORONARY ARTERY DISEASE due to recurrent ischemia to the heart and infarction which kill the vessels in the heart and make the heart thin and dilated too large and weak. The other common cause of CHF in older ppl but not until they're very old is HTN leading to thickening of the heart bc the heart to work hard to push the BP so it gets bigger and thicker and the ventricle cavity smaller. And, they have diastolic or systolic HF? DIASTOLIC. Why diastolic HF? Why? bc it's too thick and it cannot dilate. It's old heart and it's thick. Main issue is poor diastolic function. This is a particular common cause in pt who's older and long-standing HTN. So, if 88 y/o women comes to clinic with HF and she never smokes and she hasn't had many medical problems all her life. She's probably has diastolic HF. If 48 y/o african american man, who eats meat smokes and drinks gambles and does drugs doesn't take care of himself and comes to ur clinic and hospitalized, coronary artery disaese HF, primarily systolic HF bc the heart is too thin so it cannot pump.
PE: edema in legs. Hears fluid in the lungs (crackles).
~bf
COPD
COPD usually caused by smoking. COPD = chronic obstructive pulmonary disease. Chronic means >6mo. Obstructive means there's a blockage. Pulmonary means the lungs. So, COPD is the obstructive dz of the lungs. We used to call it emphysema = damage of the alveoli, they are very thin. They don't have much air exchange. They kinda thin out and they get bigger. Lungs is like sponge = tiny little holes and pockets for air to move around. It looks like sponge. It should look like a sponge. COPD lungs are mostly air. And, that's bad. We don't want lungs to be full of air. The lungs should be a sponge. COPD lungs and chest x-ray, it's much more overinflated and clear. U should be able to see it on CXRAY. It's going to look more black.
They also used to be chronic bronchitis. Chronic inflammation of the bronchi. They get narrowed and they get full of junk and they get narrower and they get infxn. They can have some phlegm and coughing and can be like asthma.
When the pt is having a very difficulty time breathing and they try to exhale, it doesn't work. And, that doesn't work. You'll see pt trying to breathe out slowly. They have prolonged expiratory phase. They breathe out very long and slowly with their mouth closed. That's what they call purse lip breathing. They do this to compensate for obstructive bronchi.
Now we know that it's not one thing or another. Most pt have emphysema or chronic bronchitis. Most ppl have features of both. So, hyper-inflated lungs, difficulty breathing, coughing, more infxn, chronic. Do their lungs get oxygen better or worse? Worse? Because damage of alveoli and obstructive bronchi. What's their pulse ox going to be ? Less than normal.
PE: no fluid sounds in lungs (no crackles). but hyper-resonating sounds (egophony).
They also used to be chronic bronchitis. Chronic inflammation of the bronchi. They get narrowed and they get full of junk and they get narrower and they get infxn. They can have some phlegm and coughing and can be like asthma.
When the pt is having a very difficulty time breathing and they try to exhale, it doesn't work. And, that doesn't work. You'll see pt trying to breathe out slowly. They have prolonged expiratory phase. They breathe out very long and slowly with their mouth closed. That's what they call purse lip breathing. They do this to compensate for obstructive bronchi.
Now we know that it's not one thing or another. Most pt have emphysema or chronic bronchitis. Most ppl have features of both. So, hyper-inflated lungs, difficulty breathing, coughing, more infxn, chronic. Do their lungs get oxygen better or worse? Worse? Because damage of alveoli and obstructive bronchi. What's their pulse ox going to be ? Less than normal.
PE: no fluid sounds in lungs (no crackles). but hyper-resonating sounds (egophony).
atelectasis
it can be normal or it can be severe or bad. A lot of time some atelectasis is normal if you've been in bed all day and not getting around. That's why you need the pt to take a deep breath a couple times before you do the pulse ox. If they've been in bed all day, have them take a couple of breaths to clear out atelectasis. Atelectasis has nothing to do smoking. It's usually due to pt staying in bed all day.
Subscribe to:
Posts (Atom)


















.jpg)
